Hospital-acquired (nosocomial) pneumonia is defined as pneumonia occurring 48 hours or more after admission (35). Bacteria are the most frequently identified cause. The most common organisms early in the hospital course (within the first 4 days) are S. pneumoniae, Moraxella catarrhalis, S. aureus, and H. influenzae (36). Most pneumonias that develop 5 or more days after hospitalization are caused by enteric gram-negative organisms, most commonly Enterobacter species, Escherichia coli, Klebsiella species, and Proteus species, or by S. aureus (35). Pneumonia is particularly common after surgery and in patients undergoing mechanical ventilation. Pneumonia may occur in up to 18% of patients who have undergone surgery (37) and up to 25% to 50% of patients undergoing mechanical ventilation (38,39,40). Nosocomial bacterial pneumonia is often difficult to recognize because the clinical criteria are nonspecific and bilateral areas of consolidation are often present secondary to acute respiratory distress syndrome (ARDS). In one investigation, nosocomial bacterial pneumonia was found histologically at autopsy in 58% of patients with ARDS, in 36% of whom it was unsuspected (41).
The etiology of nosocomial pneumonia is influenced by the presence of specific risk factors. For example, anaerobic bacteria are more likely to be found in patients who develop pneumonia after aspiration or who have poor dentition or altered consciousness (42). Pseudomonas aeruginosa infection should be considered in patients who have received corticosteroids or broad-spectrum antibiotics, who have had a prolonged stay in the ICU, or who have underlying bronchiectasis (43). Prolonged hospitalization or prior use of antibiotics also favors the development of nosocomial pneumonia caused by antibiotic-resistant organisms, such as methicillin-resistant S. aureus, Acinetobacter species, Serratia marcescens, and P. aeruginosa (44).
Radiologic Manifestations of Bacterial Pulmonary Infection
Bacterial pulmonary infection is usually acquired through the tracheobronchial tree, most commonly by aspiration
or inhalation of microorganisms, or, occasionally, by direct physical implantation from an infected source, such as a bronchoscope (
45). Pulmonary infection may also occur through the pulmonary vasculature, typically in association with an extrapulmonary focus of infection such as endocarditis. The organisms responsible for the infection may be found free in the blood (sepsis) or may be associated with thrombus (septic emboli).
Bacteria result in two main types of pneumonia: Lobar (nonsegmental) pneumonia and bronchopneumonia (lobular pneumonia). Other manifestations include abscess formation, pneumatocele, septic embolism, pleural effusion, and empyema.
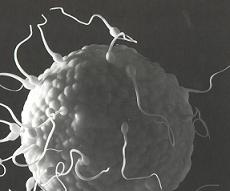
Lobar (nonsegmental) pneumonia is characterized histologically by the filling of alveolar airspaces by an exudate of edema fluid and neutrophils (see Fig. 2.1) (46). The consolidation usually begins in the periphery of the lung adjacent to the visceral pleura and spreads centripetally through interalveolar pores (pores of Kohn) and small airways (46). The airspace filling typically extends across pulmonary segments (nonsegmental consolidation), sometimes to involve the entire lobe (see Fig. 2.2). Lobar pneumonia is characterized on the radiograph and on computed tomography (CT) scan by the presence of homogeneous airspace consolidation involving adjacent segments of a lobe (see Fig. 2.3 and Table 2.1). The consolidation tends to occur initially in the periphery of the lung beneath the visceral pleura and usually abuts an interlobar fissure. The consolidation spreads centrally across segmental boundaries and may eventually involve the entire lobe. The bronchi usually remain patent, resulting in air bronchograms within the areas of consolidation. On high-resolution CT scan, areas of ground-glass opacities denoting incomplete filling of alveoli can often be seen adjacent to the airspace consolidation (see Fig. 2.4) (47,48). Most cases of lobar pneumonia are caused by bacteria, most commonly by S. pneumoniae and less commonly by Klebsiella pneumoniae, Legionella pneumophila, H. influenzae, and M. Tuberculosis (11,49).
Bronchopneumonia (lobular pneumonia) is characterized histologically by predominantly peribronchiolar inflammation (see
Fig. 2.5) (
46). This peribronchiolar inflammation is initially reflected by the presence of a small nodular or reticulonodular pattern on the radiograph and centrilobular nodules and branching opacities (tree-in-bud pattern) on high-resolution CT scan (see
Fig. 2.6). Further extension into the adjacent parenchyma results in patchy airspace nodules (centrilobular lesions with poorly defined margins measuring 4 to 10 mm in diameter) (see
Figs. 2.6 and
2.7) (
46,
50,
51). These small foci of disease may
progress to lobular, subsegmental, or segmental areas of consolidation (see
Figs. 2.6 and
2.8 and
Table 2.2). The areas of consolidation may be patchy or confluent, involve one or more segments of a single lobe, and may be multilobar, unilateral, or bilateral (
51). Confluence of pneumonia in adjacent lobules and segments may result in a pattern simulating lobar pneumonia; distinction from the latter can be made in most cases by the presence of segmental or lobular distribution of the abnormalities in other areas. Cavitation is common particularly in patients with extensive consolidation (
22). Because it involves the airways, bronchopneumonia frequently results in loss of volume of the affected segments or lobes. Air bronchograms are seldom evident on the radiograph but can frequently be seen on high-resolution CT scan.
Characteristic manifestations of bronchopneumonia on high-resolution CT scan include centrilobular nodules and branching linear opacities, airspace nodules, and multifocal lobular areas of consolidation (see Fig. 2.9) (46,47,48). The nodular and branching linear opacities result in an appearance resembling a tree-in-bud and reflect the presence of inflammatory exudate in the lumen and walls of membranous and respiratory bronchioles and the lung parenchyma immediately adjacent to them (46). The nodules seen in bronchopneumonia usually measure 4 to 10 mm in diameter and have poorly defined margins. Although these nodular opacities are often referred to as “acinar shadows,†they reflect the presence of peribronchiolar areas of consolidation and not acinar consolidation (46,50). Therefore the term airspace nodules is preferable. The most common causative organisms of bronchopneumonia are S. aureus, H. influenzae, P. aeruginosa, and anaerobic bacteria (11,22,47).
It should be noted that the radiologic pattern is influenced by the presence of underlying disease such as emphysema and age, and immunologic status of the patient (52). It is also important to keep in mind that the radiographic manifestations are often delayed. This is particularly important in nosocomial infections in patients whose chest radiographs are often performed within hours of the onset of symptoms, a time when the pneumonia may not yet be apparent on the radiograph (22). Radiographic abnormalities may be particularly delayed in patients with neutropenia (53). In one study of 175 consecutive patients with gram-negative pneumonia who were neutropenic following antineoplastic chemotherapy, 70 episodes of pneumonia were initially diagnosed clinically, in the absence of radiographically detectable disease (53). In 27 of these 70 episodes, pneumonia was evident on a follow-up radiograph. In 25 of 57 patients with no radiographically detectable infiltrates, the diagnosis of pneumonia was established at autopsy (53). The radiographic appearance of a visible pneumonic infiltrate may be delayed not only in patients with neutropenia but also in those with functional defects of granulocytes due to diabetes, alcoholism, and uremia (22). CT scan, particularly high-resolution CT scan, has been shown to be more sensitive than the radiograph in the detection of subtle abnormalities and may show findings suggestive of pneumonia up to 5 days earlier than chest radiographs (54).
High-resolution CT scan allows a better depiction of the pattern and distribution of pneumonia than the radiograph (48,55) but is seldom required in the evaluation of patients with suspected or proved bacterial pneumonia. CT scan is recommended, however, in patients with clinical suspicion of infection and normal or nonspecific radiographic findings, in the assessment of suspected complications of pneumonia or suspicion of an underlying lesion such as pulmonary carcinoma (22,56). CT scan is also indicated in patients with pneumonia and persistent or recurrent pulmonary opacities (22).
Lung abscess is defined as a localized necrotic cavity containing pus (
57). It usually represents an inflammatory mass, the central part of which has undergone purulent liquefactive necrosis (
11). The most common cause of lung abscess is aspiration (
57). Abscesses occur most commonly in the posterior segment of an upper lobe or the superior segment of a lower lobe (
57). However, they may also be present predominantly or exclusively in the anterior lung regions (see
Fig. 2.10). Lung abscesses usually measure 2 to 6 cm in diameter, although they may become larger measuring up to 12 cm in diameter (
57). Abscesses often
erode into an airway, resulting in drainage of necrotic material and the formation of a cavity (see
Fig. 2.10). Pulmonary abscesses may develop in the course of known pneumonia or may be the initial manifestation of the disease. The radiologic manifestations consist of single or multiple masses that are often cavitated (see
Table 2.3). In one review of the radiographic findings in 50 patients, the internal margins of the abscesses were smooth in 88% and shaggy in 12% (
58). Air–fluid levels were present in 72% and adjacent parenchymal consolidation in 48%. Maximal wall thickness was equal to or <4 mm in 4% of cases, between 5 and 15 mm in 82%, and >15 mm in 14%. CT scan typically demonstrates low-attenuation central region or cavitation and rim enhancement following intravenous administration of contrast (
Fig. 2.10) (
59,
60). Common causes of lung abscess include anaerobic bacteria (most commonly
Fusobacterium nucleatum and Bacteroides species),
S. aureus, P. aeruginosa, and
K. pneumoniae (
57,
61).
Occasionally pneumonia may result in extensive necrosis (necrotizing pneumonia). Radiologic manifestations
consist initially of small lucencies within an area of consolidated lung, usually developing within lobar consolidation associated with enlargement of the lobe and outward bulging of the fissure (bulging fissure sign) (
62) (see
Fig. 2.11). The lucencies rapidly coalesce into a large cavity containing fluid and sloughed lung (see
Fig. 2.12).
Pneumatocele is a thin-walled, gas-filled space that usually develops in association with infection (11). It presumably results from drainage of a focus of necrotic lung parenchyma followed by check-valve obstruction of the airway subtending it, enabling air to enter the parenchymal space during inspiration but preventing its egress during expiration (63). The complication is caused most often by S. aureus in infants and children and Pneumocystis jiroveci in patients who have acquired immunodeficiency syndrome (AIDS) (52,64). Pneumatoceles typically increase in size over days or weeks, may result in pneumothorax, and usually resolve over weeks or months (see Fig. 2.13).
Septic emboli to the lungs originate in a variety of sites, including cardiac valves (endocarditis), peripheral veins (thrombophlebitis), and venous catheters or pacemaker wires. The common feature in all these sites is endothelial damage associated with the formation of friable thrombus-containing organisms (usually bacteria) (52). Turbulence of flowing blood results in the detachment of small fragments of thrombus that are carried to the pulmonary arteries. Septic embolism is characterized radio-logically by the presence of nodules that usually measure 1 to 3 cm in diameter and that are frequently cavitated (see Fig. 2.14). The cavitation reflects the necrosis associated with the organisms and the neutrophilic exudate. On cross-sectional CT images the nodules often appear to have a vessel leading into them. This has been called the feeding vessel (see Fig. 2.15) (65,66). Multiplanar and maximum intensity projection (MIP) reformations have shown however that in most patients the pulmonary arteries course around the nodule and that vessels appearing to enter the nodule usually are pulmonary veins draining the nodule (Fig. 2.15) (67). Dodd et al. performed multidetector high-resolution CT scan in 14 patients with septic embolism (67). Ninety-three nodules (40%) showed a vessel that appeared to enter the nodule on transverse images, but the vessel was shown to pass around the nodule on multiplanar reconstructions and/or MIPs. Forty-four nodules (19%) showed a central vessel entering the lesion on all imaging planes. All of these vessels could be traced back to the left atrium on transverse images, consistent with pulmonary vein branches. The “feeding vessel†sign is therefore a misnomer and is of limited value in the diagnosis of septic embolism.
Occlusion of pulmonary arteries by septic emboli or thrombus may result in hemorrhage and/or infarction and less well-defined or wedge-shaped foci of disease. These subpleural wedge-shaped areas of consolidation,
often with central areas of necrosis or frank cavitation, are often difficult to identify on the radiograph but are commonly seen on CT scan (
66). Septic emboli are seen most commonly in intravenous drug users and in patients with central venous lines.